- Understanding Cataracts: Causes, Symptoms, and Treatment
What Do You Understand By Cataract ?
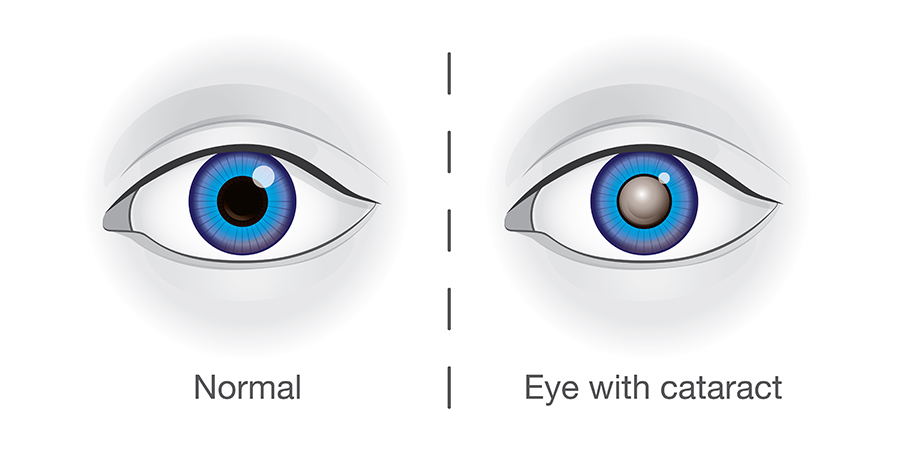
A cataract is an eye condition that is characterized by the clouding of the natural lens in the eye, which leads to vision loss. Naturally, the eye’s lens is clear and allows light to pass through, focusing on the retina at the back of the eye. However, when a cataract develops, the lens becomes cloudy, and this cloudiness interferes with the normal passage of light.
Cataracts: What They Are, How They Affect Your Vision, and How Modern Treatment Can Restore Your Sight
Most cataracts develop in people over age 55, but they occasionally occur in infants and young children or as a result of trauma or medications. Usually, cataracts develop in both eyes, but one may be worse than the other.
The lens is located inside the eye behind the iris, the colored part of the eye. Normally, the lens focuses light on the retina, which sends the image through the optic nerve to the brain. However, if the lens is clouded by a cataract, light is scattered so the lens can no longer focus it properly, causing vision problems. The lens is made of mostly proteins and water. The clouding of the lens occurs due to changes in the proteins and lens fibers.
Types of cataracts
The lens is composed of layers, like an onion. The outermost is the capsule. The layer inside the capsule is the cortex, and the innermost layer is the nucleus. A cataract may develop in any of these areas. Cataracts are named for their location in the lens:
- A nuclear cataract is located in the center of the lens. The nucleus tends to darken with age, changing from clear to yellow and sometimes brown.
- A cortical cataract affects the layer of the lens surrounding the nucleus. The cataract looks like a wedge or a spoke.
- A posterior capsular cataract is found in the back outer layer of the lens. This type often develops more rapidly.
Causes & risk factors
Most cataracts are due to age-related changes in the lens of the eye that cause it to become cloudy or opaque. However, other factors can contribute to cataract development, including:
- Diabetes mellitus. People with diabetes are at higher risk for cataracts.
- Drugs. Certain medications are associated with cataract development. These include:
- Corticosteroids.
- Chlorpromazine and other phenothiazine related medications.
- Ultraviolet radiation. Studies show an increased chance of cataract formation with unprotected exposure to ultraviolet (UV) radiation.
- Smoking. There is possibly an association between smoking and increased lens cloudiness.
- Alcohol. Several studies show increased cataract formation in patients with higher alcohol consumption compared with people who have lower or no alcohol consumption.
- Nutritional deficiency. Although the results are inconclusive, studies suggest an association between cataract formation and low levels of antioxidants (for example, vitamin C, vitamin E, and carotenoids). Further studies may show that antioxidants can help decrease cataract development.
- Family History. If a close relative has had cataracts, there is a higher chance of developing a cataract.
Rarely, cataracts are present at birth or develop shortly after. They may be inherited or develop due to an infection (such as rubella) in the mother during pregnancy. A cataract may also develop following an eye injury or surgery for another eye problem, such as glaucoma.
Symptoms
Cataracts generally form very slowly. Signs and symptoms of a cataract may include:
- Blurred or hazy vision.
- Reduced-intensity of colors.
- Increased sensitivity to glare from lights, particularly when driving at night.
- Increased difficulty seeing at night.
- Change in the eye’s refractive error, or eyeglass prescription.
Diagnosis
Cataracts are diagnosed through a comprehensive eye examination. This examination may include:
- Patient history to determine if vision difficulties are limiting daily activities and other general health concerns affecting vision.
- Visual acuity measurement to determine to what extent a cataract may be limiting clear distance and near vision.
- Refraction to determine the need for changes in an eyeglass or contact lens prescription.
- Evaluation of the lens under high magnification and illumination to determine the extent and location of any cataracts.
- Evaluation of the retina of the eye through a dilated pupil.
- Measurement of pressure within the eye.
- Supplemental testing for color vision and glare sensitivity.
Further testing may be needed to determine how much the cataract is affecting vision and to evaluate whether other eye diseases may limit vision following cataract surgery.
Using the information from these tests, your doctor of optometry can determine if you have cataracts and advise you on your treatment options.
Cataract Treatment Procedure: Phacoemulsification (Phaco)
Phacoemulsification, commonly known as phaco, is the most advanced and widely preferred technique for cataract surgery. This modern method is renowned for its precision, safety, and minimal recovery time, making it the gold standard in cataract treatment.
Step-by-Step Phacoemulsification (Phaco) Surgery:
Creating a Small Incision:
The procedure begins with the surgeon making a very small incision, typically about 2-3 millimeters, at the edge of the cornea, which is the transparent outer layer of the eye. This tiny incision is carefully crafted to ensure minimal disruption to the eye structure and to facilitate faster healing.
Insertion of the Ultrasound Probe:
Through this small incision, a thin probe is inserted into the eye. This probe is a high-frequency ultrasound device that emits ultrasonic waves. These waves are specifically designed to soften and break up the cataract-affected lens into tiny fragments, a process known as emulsification.
Suctioning Out the Lens Fragments:
Once the lens has been emulsified, the tiny fragments are gently suctioned out of the eye using the same probe. This step effectively removes the cloudy lens material that has been causing blurred or impaired vision.
Implantation of the Artificial Intraocular Lens (IOL):
After the cataract has been fully removed, a foldable artificial intraocular lens (IOL) is implanted through the same small incision. The IOL is carefully positioned to replace the natural lens, restoring clear and sharp vision. Modern IOLs are designed to be permanent, requiring no maintenance, and can even provide enhanced focusing abilities, mimicking the natural lens.
Completion and Recovery:
The small incision made during the procedure is typically self-sealing and usually does not require stitches. This contributes to a quicker recovery process, allowing patients to experience significant improvements in vision within a short period. Most patients can resume their normal activities soon after the surgery, with minimal restrictions.
Benefits of Phacoemulsification:
- Minimally Invasive: The small incision size reduces the risk of complications and promotes faster healing.
- Rapid Recovery: Patients often notice an improvement in their vision almost immediately, with full recovery occurring within a few weeks.
- High Success Rate: Phacoemulsification is one of the safest and most effective surgeries, with the vast majority of patients experiencing significantly improved vision.
Prevention
There is no treatment to prevent or slow cataract progression. In age-related cataracts, changes in vision can be very gradual. Some people may not initially recognize the visual changes. However, as cataracts worsen, vision symptoms increase.
While there are no clinically proven approaches to preventing cataracts, simple preventive strategies include:
- Reducing exposure to sunlight through UV-blocking lenses.
- Decreasing or stopping smoking.
Increasing antioxidant vitamin consumption by eating more leafy green vegetables and taking nutritional supplements.
- QUESTION AND ANSWER
General Frequently Asked
Question For Abour Us
Certainly! Here’s how you could structure the General Frequently Asked Questions (FAQ) content for an “About Us” section on a website:
A cataract is a condition where the natural lens of the eye becomes cloudy, leading to blurred vision and difficulty with daily activities like reading or driving.
Symptoms of cataracts include blurred or foggy vision, difficulty seeing at night, sensitivity to light, seeing halos around lights, and a need for brighter light when reading. If you experience any of these symptoms, it’s advisable to schedule an eye examination.
Cataract surgery is usually recommended when your vision becomes significantly impaired and begins to affect your daily activities, such as reading, driving, or recognizing faces. Your ophthalmologist will guide you on the best time for surgery.
Cataract surgery involves removing the cloudy lens and replacing it with a clear artificial lens, known as an intraocular lens (IOL). The most common and advanced method is phacoemulsification, which is minimally invasive and allows for a quick recovery.
Cataract surgery is generally not painful. It is performed under local anesthesia, which numbs the eye, so you won’t feel any pain during the procedure. Some patients may experience mild discomfort or a gritty feeling after surgery, but this usually subsides within a few days.
Recovery from cataract surgery is typically quick. Most patients notice improved vision within a few days, and full recovery usually occurs within a few weeks. You may be advised to avoid strenuous activities and protect your eye from potential irritants during the recovery period.
Many patients experience significantly improved vision after cataract surgery, and some may not need glasses for distance vision. However, you may still need reading glasses or glasses for certain tasks, depending on the type of intraocular lens implanted and your individual vision needs.
Cataract surgery is one of the safest surgical procedures, but like any surgery, it carries some risks, including infection, bleeding, or retinal detachment. Your ophthalmologist will discuss these risks with you and take steps to minimize them.
Before surgery, your ophthalmologist will perform a thorough eye examination and measure your eye to determine the correct lens implant. You may be advised to stop taking certain medications or apply eye drops before surgery.
If you have any concerns or questions about cataract surgery, it’s important to discuss them with your ophthalmologist. They can provide detailed information and address any specific worries you may have.

